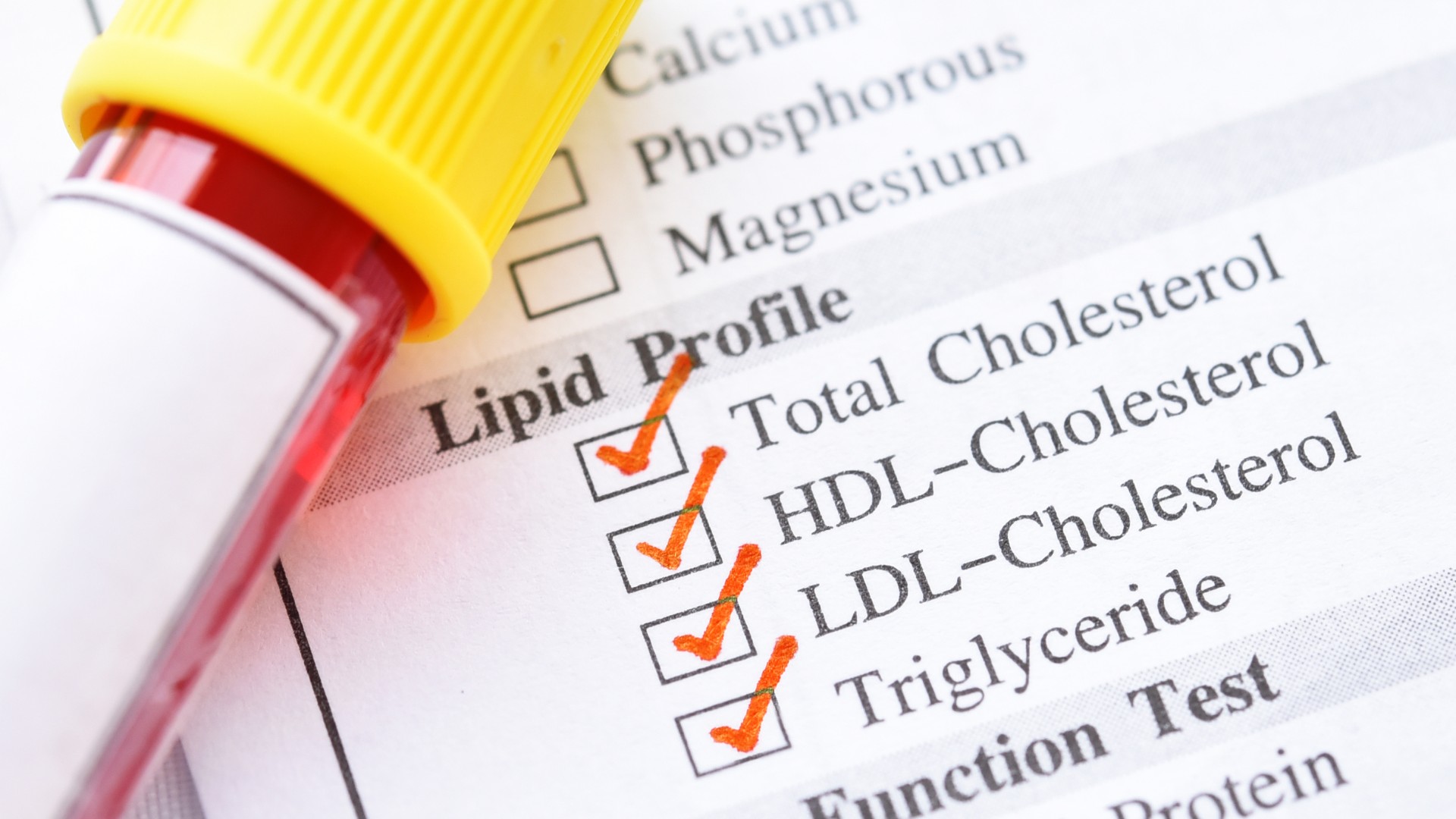
Laboratory testing of blood lipid levels is a routine examination in the doctor's office. LDL cholesterol and HDL cholesterol are determined most frequently. But what do these values tell us? What is the story behind "bad" and "good" cholesterol? Why are blood lipid levels an important cornerstone of your longevity and why does Dr. Peter Attia devote an entire chapter to this topic in his new book? You can find out all this in this article.
Background - where do blood lipid levels come from?
In order to better understand the laboratory values, it is worth taking a closer look at our own fat metabolism, also known as lipid metabolism. Fats are distributed throughout the body and occur in different forms. They form as phospholipids They are the basis for the synthesis of various hormones, such as cortisol or testosterone, and serve as energy stores in the form of triglycerides. We absorb fatty acids daily through our intestines with our food and then distribute the individual molecules to every corner of our body with the help of the blood - ideally to where they are actually needed. The right composition of fatty acids and a sufficient supply of omega-3 fatty acids.

Did you know? Phospholipids are not only found in the cell membranes of our body. They are also found in chocolate, ice cream, margarine and cosmetic products. In medicine, they are used as a component of food supplements to increase bioavailability.
You can see the effect this use can have using the example of Quercesome. The specially formulated quercetin C complex from MoleQlar is around 20 times more bioavailable than conventional quercetin powder. The key players here are phospholipids from sunflowers and the clever combination with natural vitamin C - a bio-enhancer of quercetin. With Berbersome - the berberine mineral complex from MoleQlar - the increase in berberine bioavailability due to phospholipids is 10-fold.
Fat and water - the transport challenge
From a chemical point of view,fats are not soluble in water (hydrophobic). This phenomenon can be easily recognized by adding a few drops of oil to water. The oil does not mix with the water, but floats on the surface in the form of drops. So how does our body do this when blood is also largely made up of water? So-called apolipoproteins exist to overcome this challenge. These enclose the fatty acids and form a water-soluble (hydrophilic) shell. You can imagine the whole thing as a small sphere. The water-soluble proteins are on the outside and the water-insoluble fats are on the inside. Apolipoproteins and fatty acids together are also known as lipoproteins and form the basis for laboratory measurements of fat metabolism.
Which blood lipid values can be measured?
Lipoproteins are classified into different categories based on their density. The following parameters are usually measured:
- LDL cholesterol
- HDL cholesterol
- Total cholesterol
- Triglycerides
- Non-HDL cholesterol
In some laboratory findings, these two values also appear:
- ApoB
- Lp(a)
In Germany, blood lipid levels in healthy adults are usually examined once as part of the health check-up. From the age of 35, blood lipid levels can be checked every three years. In the neighboring country to the south, Austria, the statutory health insurance funds are somewhat more generous. Here, an annual laboratory examination is possible as part of the preventive medical checkup.
What are the standard values of blood lipids?
The standard values vary depending on age and personal risk. The European Society of Cardiology (ESC) defines the following thresholds for people under 65 at low risk:
| Total cholesterol | <190 mg/dL (5mmol/L) |
| HDL cholesterol | In men >40 mg/dL (1mmol/L)
In women >45 mg/dL (1.2mmol/L) |
| Non-HDL cholesterol | <145 mg/dL (3,8mmol/L) |
| LDL cholesterol | <115 mg/dL |
| apoB | <100 mg/dL (1,0mmol/L) |
| Lp(a) | <50 mg/dL |
| Triglycerides | Nüchtern: <150 mg/dL (1,7mmol/L)
Nicht-Nüchtern: <175 mg/dL (2,0mmol/L) |
Did you know? In patients with far too many fatty acids in the blood, a condition known as hypertriglyceridemia, this can sometimes be seen with the naked eye. When the patient's blood is separated into liquid (serum) and solid blood components (cells) using a centrifuge, the serum looks milky white. Normally, the serum is clear and yellow in color.
Triglycerides - more than just fat
Triglycerides do not directly contribute to vascular calcification. For this reason, they are not always given enough attention. But triglyceride levels are just as important for your longevity.
Values above 800 mg/dL, for example, can trigger pancreatitis at any time. And even though triglycerides, unlike LDL, cannot deposit directly in the vessel wall, they do have an indirect effect on atherosclerosis via IDL particles (more on this later). For this reason, your triglyceride levels should not exceed the limits mentioned above.
In addition to exercise and a healthy, Mediterranean diet, the ESC mentions two supplements that can lower triglyceride levels. One of these is berberine, which has been shown in studies to lower both LDL cholesterol and triglycerides. In MoleQlar, berberine is available in phospholipid form, which has 10 times better bioavailability than normal berberine powder.
Blood lipid levels: The myth of "good" and "bad" cholesterol
If you want to have your blood lipid levels determined, doctors will usually measure your total cholesterol, your HDL cholesterol, your LDL cholesterol and your triglycerides. Often, as a patient, you'll hear phrases like, "Your bad cholesterol (LDL) is a little high, but your good cholesterol (HDL) balances thatout." Metaphors like "you better lay off that" (LDL) and "love you" (HDL) are also common. Or you're just told your blood lipids are normal. But what does normal actually mean, and why is the good and bad cholesterol thing just a fairy tale?
To understand this in more detail, we need to take another look at cholesterol metabolism. Cholesterol is absolutely vital for our body. Put simply, it is a special fat molecule that we need for every cell in our body. Very abbreviated, you can imagine the cholesterol metabolism like this:
- Cholesterol is produced in the liver. The endogenous cholesterol, triglycerides and apolipoproteins are then combined. This is how VLDL particles (very-low-density-lipoproteins) are formed.
- These VLDL molecules are quite large and are now transported with the blood.
- In the body, these VLDL molecules release triglycerides (for example to muscle cells) and thus become smaller. They are now called VLDL remnants or IDL molecules.
- The more cholesterol or triglycerides the VLDLs release, the smaller they become. Via the intermediate stage of IDLs, they eventually become the familiar LDL molecules.
- The LDL molecules can ultimately be taken up by cells via receptors. These are located, for example, in the liver, muscle cells or lipid cells.
- HDL molecules have a different purpose. If too much cholesterol accumulates outside the liver, HDL collects it and transports it back to the liver.
The cholesterol eggs falsehood
Cholesterol occurs naturally in our food (eggs in particular are rich in cholesterol). However, the majority of our cholesterol in the blood is produced by ourselves. It is therefore called endogenous or the body's own cholesterol. Exogenous, externally supplied cholesterol, contributes very little to the increase in cholesterol levels.
For a long time, the belief persisted that eggs would lead to a sharp increase in LDL levels and thus to a higher risk of cardiovascular disease. Recent studies have shown that eggs do cause a slight increase in LDL, but from a subgroup of LDL molecules that are too large to be deposited in the vascular wall. Thus, eggs are healthier than thought, because they contain heaps of vitamins and other healthy substances. (Blesso & Fernandez, 2018)

The moral of the story? A functioning organism needs all forms of cholesterol molecules. LDL transports vital cholesterol from the liver to the other regions of the body, and HDL can retrieve excess cholesterol. If, on the other hand, there is an excess of LDL or an imbalance of LDL/HDL, this first leads to vascular deposits and, over a long period of time, to arteriosclerosis.
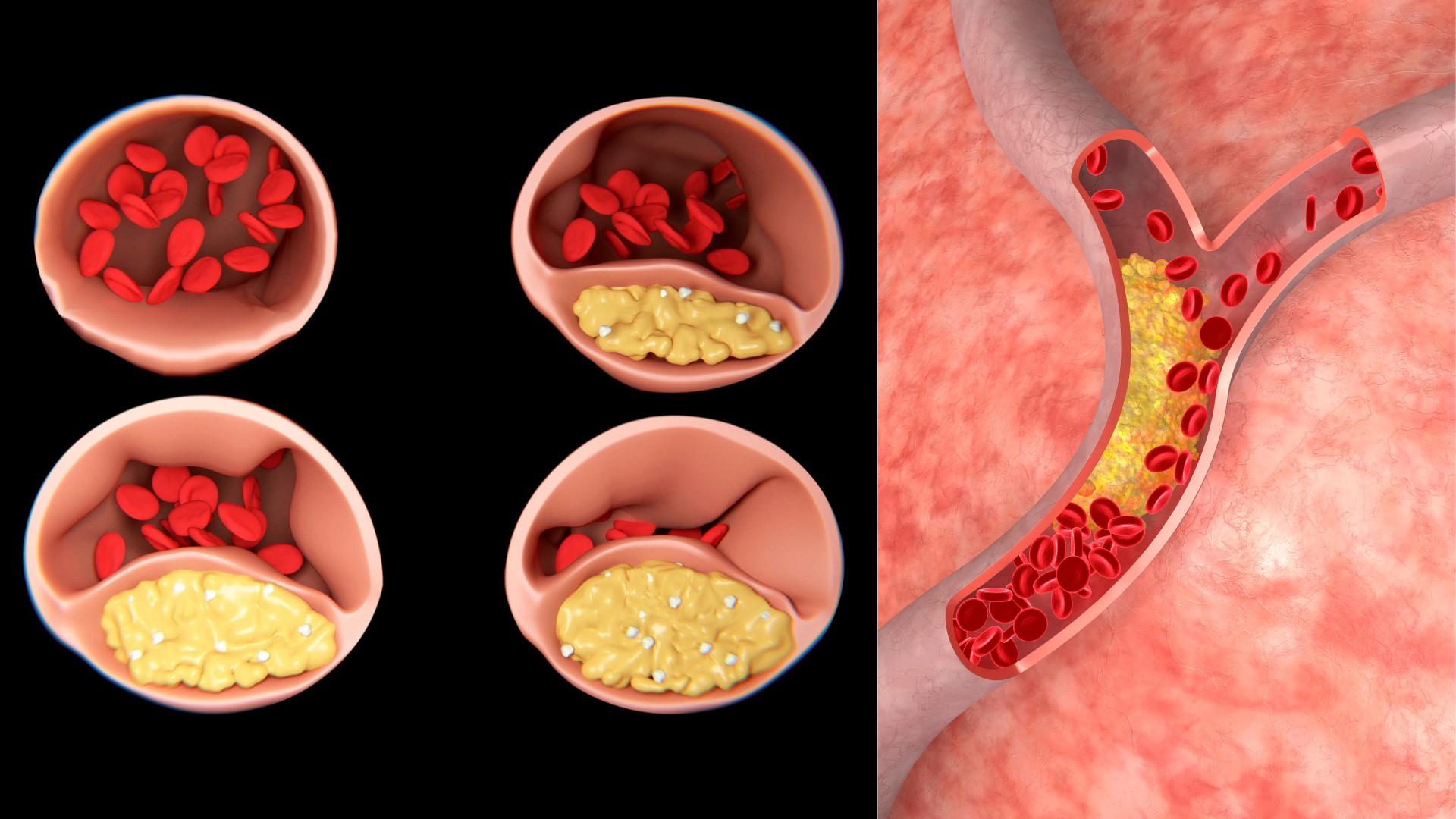
Arteriosclerosis - the number one killer in the western world
Arteriosclerosis - also known colloquially as vascular calcification - is a silent killer. Over decades, small fat molecules are deposited in the walls of our blood vessels, which gradually become larger and larger. This leads to inflammatory reactions, plaque formation and ultimately to the narrowing of entire blood vessels. You usually only notice arteriosclerosis when a vessel is almost completely blocked. The result is a lack of oxygen in the supplied tissue (ischemia). People with severely "calcified" coronary arteries can feel "ischemia pain" when they exert themselves. The vessels are too narrow for the blood due to the "calcifications". This leads to an undersupply of oxygen and those affected notice a stabbing pain in the chest. In the worst case scenario, a heart attack or stroke can occur if parts of the plaque become detached, blocking entire vessels. (Khatana et al., 2020)
Did you know? When we talk about vascular calcification, we often mean the fatty deposits caused by LDL particles. However, it is not only LDL that plays a role, but also calcium. Too much calcium in the blood vessels can lead to significantly more "calcification". This is counteracted by Vitamin K2. Several studies have shown that vitamin K2-dependent proteins can reduce vascular calcification. (Halder et al., 2019)
According to one of the world's largest studies (Global Burden of Disease), published in the Journal of the American College of Cardiology, cardiovascular disease, which includes atherosclerosis, is the leading cause of death worldwide. Millions of people die from it each year. The authors estimate that up to one-third of the population worldwide dies from cardiovascular disease, and atherosclerosis is one of the major contributors. (Roth et al., 2020)

High LDL levels are a modifiable risk factor for cardiovascular disease. This is where the colloquial term "bad" cholesterol came from. However, it is only in recent years that researchers have discovered why this is too short-sighted.
In addition to high LDL levels, high blood pressure and high blood sugar are at least as big risk factors. You can find out what insulin resistance is and why it is so important for your longevity in our article on insulin resistance .
Why is LDL cholesterol measurement so important - and at the same time prone to error?
Quick heads up, in this section we need to dive a little deeper into some studies. Admittedly, the topic is complex, but by the end of this section, hopefully it will be clear why measuring LDL cholesterol alone is not enough for you.
LDL is one of the main factors in the development of atherosclerosis. In healthy adults, the value should not exceed 115mg/dL.
Imagine for a moment that your blood vessel walls are not a perfectly tight tube. Instead, they are full of tiny "holes" that we need to allow nutrients and cells to move freely between our blood system and other compartments of our body.
The LDL particles are so small that they can push through our blood vessel walls. HDL molecules, on the other hand, are too large and cannot enter the vessel wall. When passing through the vessel wall, small errors naturally occur, meaning that an LDL molecule does not get through the perforated wall in your blood vessel and gets "stuck". If this happens too often, "vascular calcification" occurs via complex remodeling mechanisms. The more LDL molecules there are in your blood, the greater the risk of these "natural errors". For this reason, LDL cholesterol is used as a laboratory parameter. However, it is not only LDL molecules that have this so-called atherosclerotic effect, but also IDLs. These would not be "counted" in a measurement. This is the first "blind spot" in the measurement of LDL cholesterol. It is simply only part of the fat truth.
LDL - Estimating versus measuring
What makes the subject of blood lipid levels even more complex is the fact that there are different types of measurement. Classically, LDL cholesterol (LDL-C) is estimated using the Friedwald formula. (Martin et al., 2013). That's right, the LDL value in common laboratory findings is usually based on an estimate.
However, there is also the possibility to measure the LDL particles numerically (LDL-P). This is a direct measurement and already much more accurate. What is also missing here, however, are the other molecules, especially IDLs.
In a large review study, different measurement methods were compared with each other. (Mora et al., 2014) Concordant and discordant measured values are shown here. So what does this mean? Let's say your LDL cholesterol is an unremarkable 105mg/dl. Remember, this is estimating the cholesterol in your LDL particles. Now you can also count the LDL particles directly, then you get the LDL-P value. If this is equal to your LDL-C value, then it is called concordance. However, if your LDL-P value is significantly higher/lower, we speak of discordant values.
Discordant values are deceptive, as a "normal" LDL-C may appear in a normal routine lab, even though your LDL-P is elevated. However, your doctor would tell you, based on the findings, "Everything is fine."
But is that really the case?
In this study, it was shown that women in particular have an increased risk of mortality if they have discordant LDL levels. In addition to LDL-P values, apoB and non-HDL cholesterol were also compared as a measurement method. For all three parameters for blood lipid levels, discordant values were associated with a higher risk compared to LDL-C.
Briefly summarized: Measuring LDL cholesterol alone may suggest a false sense of security because of the method of measurement.
ApoB - the better measurement value than LDL?
We have seen that measuring LDL cholesterol alone, using the estimation formula, simply does not give us enough information. For this reason, in his book "Outlive: The Science and Art of Longevity", Dr. Peter Attia, among others, advocates a different measurement for blood lipid levels: ApoB
ApoB is an apolipoprotein - that is, a complex of fatty acids and a water-soluble shell, if you remember the introduction. ApoB binds triglycerides and cholesterol to make them water soluble. The genius of ApoB is that every lipoprotein (except HDL) has exactly one molecule of ApoB. ApoB can therefore be used to determine much more precisely how many lipoproteins are in our bloodstream. For this reason, Longevity physician Dr. Attia advocates more focus on determining ApoB.
The role of ApoB has been known in the scientific community for some time and has been described in a review by Dr. Sniderman and others. (Sniderman et al., 2019)
The European Society of Cardiology also recognizes the role of ApoB in their 2019 guidelines and currently recommends it as an additional diagnosis in high-risk patients.
Should we measure ApoB in all people?
Should everyone now have their apoB mirror measured? This is currently still up for debate. On the one hand, proponents argue that one can assess the risk for cardiovascular diseases much better with this value. On the other hand, it is argued that LDL-C is sufficient because it is more than 90% responsible for the underlying "vascular calcification".
Low ApoB levels are usually associated with a low probability of cardiovascular disease. It can therefore make sense to determine one's level and to base one's therapy on it.
Besides apoB, there is another risk factor that indicates a high risk of atherosclerosis. We are talking about Lp(a).
Lp(a): a familial risk factor
Lp(a) (pronounced lipoprotein small a) is a genetic risk factor. People with high levels of Lp(a) have a significantly increased risk of cardiovascular disease, independent of LDL cholesterol and ApoB. Lp(a) has similar properties to LDL, so it rapidly deposits into the vessel wall. Similar to ApoB, there is ongoing debate here about how useful measurement is for everyone in the population.

Blood lipid levels - the lower the better?
Disclaimer: This article cannot give you exact medical recommendations on target values. You should always discuss these steps exclusively with your doctor!
The European Society of Cardiology has published different threshold values of LDL-C and ApoB in its guidelines. These vary greatly depending on personal risk.
The lowest LDL-C target values are around 40mg/dl and the lowest ApoB target values are below 65mg/dl. Currently, such strict limits are recommended only for people who are already severely pre-diseased.
It is currently under discussion whether an early lowering of LDL and ApoB levels, is beneficial. The idea behind this is as follows. It is now known that atherosclerosis is a slow disease that progresses over decades. Unnoticed, small fat particles are deposited in the walls of our vessels every day. If you were to cut open the vessels of those affected, you could see the "fatty plaques" with the naked eye. Such plaques, however, develop only after a long time; one also speaks of a cumulative LDL load over a lifetime.
One idea is to never reach this cumulative LDL load and thus never develop enough atherosclerosis to provoke disease. Dr. Braunwald, one of America's leading cardiologists, has even hypothesized that by lowering LDL levels early, one can live to be 100 years old without ever developing cardiovascular disease. Since cardiovascular disease is the number one cause of death, early lowering of LDL and ApoB would provide a fulminant improvement in both quality of life and life expectancy.
Literature:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7369156/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7512065/
- https://www.jlr.org/article/S0022-2275(20)34443-6/pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5946211/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4501252/#:~:text=LDL%2DP%20is%20the%20number,carried%20by%20these%20apoB%20particles.
- https://jamanetwork.com/journals/jamacardiology/article-abstract/2753612
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4226221/
- https://www.jacc.org/doi/10.1016/j.jacc.2020.11.010
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6413124
- https://www.medicoconsult.de/non-hdl-cholesterin/#:~:text=Non%2DHDL%2DCholesterin%20(Non,Risiko%20von%20Herzinfarkt%20und%20Schlaganfall.
- https://www.mdpi.com/2218-1989/11/10/690
- https://www.escardio.org/static-file/Escardio/Guidelines/publications/DYSLIPguidelines-dyslipidemias-FT.pdf
- https://pubmed.ncbi.nlm.nih.gov/22453571/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9661797/
- https://academic.oup.com/eurheartj/article/42/45/4612/6335767?login=false
Graphics:
The graphics were purchased under license from Canva.